Is Inflammation Making Your Depression Worse?
Understanding Inflammation and Its Effects
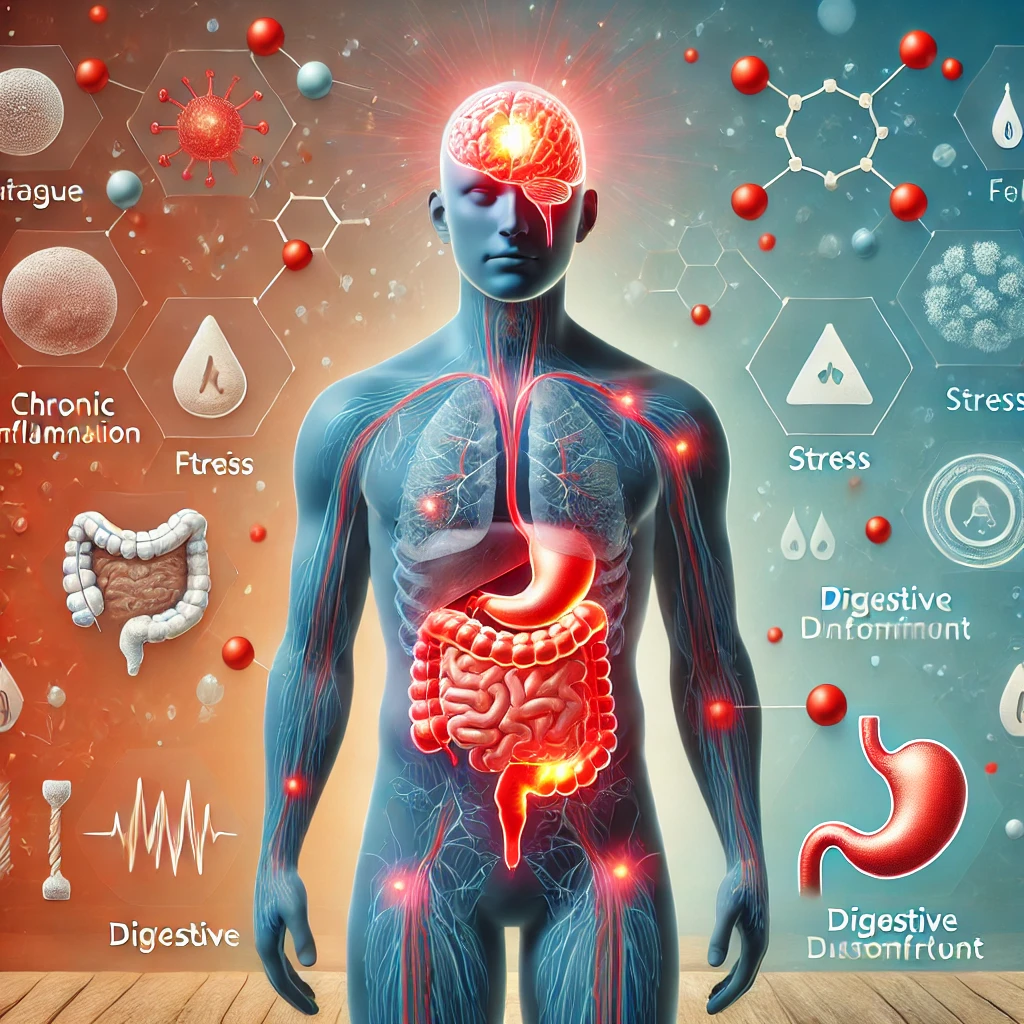
Inflammation is a natural response of the immune system, serving as a protective mechanism against harmful stimuli such as pathogens, damaged cells, and irritants. It generally manifests in two forms: acute and chronic inflammation. Acute inflammation is a short-term response, typically characterized by redness, swelling, heat, and pain, which usually resolves when the underlying cause is addressed. For instance, a cut or infection may trigger acute inflammation, leading to healing. However, when inflammation persists over an extended period, it transitions into chronic inflammation, which can lead to detrimental health effects.
Chronic inflammation can develop due to various factors, including ongoing stress, a sedentary lifestyle, poor dietary choices, obesity, and underlying health conditions such as autoimmune diseases. Diets high in processed foods, sugars, and unhealthy fats have been linked to increased inflammatory markers in the body. Furthermore, chronic stress can heighten inflammation, leading to a cycle that exacerbates mental and physical well-being. The physiological effects of chronic inflammation are particularly concerning, as it has been shown to have direct implications for brain health and functionality.
Research increasingly indicates a correlation between chronic inflammation and mood disorders, including depression. Elevated levels of pro-inflammatory cytokines can affect neurotransmitter systems, which play crucial roles in mood regulation. For instance, studies suggest that inflammation may impair serotonin production, leading to depressive symptoms. Moreover, inflammation can hinder neurogenesis, the process of forming new neurons, which is vital for cognitive flexibility and emotional resilience. Thus, understanding how chronic inflammation can impact the brain is essential for comprehending its potential role in worsening depression.
The Inflammation-Depression Connection
Recent scientific research indicates a compelling link between chronic inflammation and mood disorders, particularly depression and anxiety. Several studies have emerged over the past two decades, suggesting that elevated levels of inflammatory markers, such as C-reactive protein (CRP) and interleukin-6 (IL-6), correlate strongly with an increased incidence of depressive symptoms. For instance, a significant longitudinal study revealed that individuals with higher baseline levels of inflammatory markers were more likely to develop depression over time, indicating that inflammation may play a pivotal role in the onset and persistence of these mood disorders.
Furthermore, inflammation appears to affect key neurotransmitters, notably serotonin, which is crucial for mood regulation and often termed the “feel-good” neurotransmitter. Research has demonstrated that inflammatory cytokines can inhibit serotonin synthesis and release, thereby decreasing serotonin availability in the brain. Consequently, this disruption in serotonin levels may exacerbate depressive symptoms, leading to a vicious cycle of worsening mood and increased inflammation.
Neurobiological studies have also shown that inflammation can alter neural pathways associated with mood regulation. For instance, animal models of chronic inflammation exhibit changes in the hippocampus—a region of the brain critical for mood and emotional regulation. These alterations may contribute to cognitive dysfunctions and negative mood states found in individuals suffering from depression.
The implications of these findings are profound for those experiencing mood disorders. They emphasize the necessity of considering inflammation as a contributing factor when assessing and treating depression and anxiety. Mental health professionals might need to integrate anti-inflammatory strategies, such as dietary changes, physical activity, or pharmacological interventions, into their treatment plans, paving the way for a more holistic approach to managing mood disorders.
Natural Ways to Reduce Inflammation
Chronic inflammation has been increasingly recognized as a contributing factor to various health disorders, including mood disorders like depression. Therefore, implementing natural strategies to reduce inflammation is essential not only for physical health but also for enhancing mental well-being.
One of the most effective ways to combat inflammation is through dietary changes. Incorporating anti-inflammatory foods into one’s diet can significantly impact inflammation levels. Foods rich in omega-3 fatty acids, such as fatty fish (e.g., salmon, mackerel), flaxseeds, and walnuts, have been shown to reduce inflammatory markers in the body. Additionally, colorful fruits and vegetables are high in antioxidants, which assist in neutralizing free radicals that contribute to inflammation. Berries, spinach, and broccoli, for instance, are excellent choices that not only support immune function but also provide vital nutrients that foster better mental health.
In conjunction with including beneficial foods, it is crucial to limit the intake of processed and inflammatory foods. These typically include refined sugars, trans fats, and highly processed snacks that can exacerbate inflammation. By avoiding such items, individuals can better manage their inflammatory responses, which may, in turn, help alleviate feelings of depression.
Moreover, lifestyle changes play a pivotal role in controlling inflammation. Regular physical activity is one of the most beneficial strategies, as exercise has been shown to lower inflammation and improve mood. A combination of aerobic and strength training exercises promotes a healthy body and releases endorphins, improving overall emotional well-being.
Additionally, stress management techniques, such as mindfulness meditation, yoga, and deep-breathing exercises, can effectively mitigate stress-related inflammation. Adequate sleep is also vital; insufficient rest can lead to increased inflammatory responses. Therefore, creating a consistent sleep schedule can contribute to better inflammatory control.
Incorporating these dietary and lifestyle strategies lays a solid foundation for reducing inflammation, thus supporting improved mental health and potentially alleviating depression symptoms.
When to Seek Help
Recognizing when to seek professional help is crucial for individuals navigating the complex interplay between inflammation and depression. Symptoms of depression can often be exacerbated by bodily inflammation, leading to a cycle that is difficult to break without appropriate intervention. It is important to be aware of signs that may indicate the necessity for medical consultation. Common indicators include persistent feelings of sadness or hopelessness, significant changes in appetite or sleep patterns, and a loss of interest in daily activities.
Furthermore, physical symptoms such as chronic pain, fatigue, or digestive issues may also signify that inflammation is affecting one’s mental well-being. Individuals experiencing these symptoms should consider reaching out to healthcare providers. Mental health professionals can conduct comprehensive assessments to determine the extent of depression and its potential links to inflammation. By understanding the relationship between these two conditions, tailored treatment plans can be developed.
In practice, healthcare providers can assist in managing both inflammation and depression through a multifaceted approach that includes medications, therapy, and lifestyle modifications. Antidepressants may be prescribed to alleviate depressive symptoms while anti-inflammatory medications can target the underlying inflammation. Cognitive-behavioral therapy or other therapeutic modalities can provide coping strategies to handle emotional distress effectively.
Moreover, adopting healthy lifestyle changes—such as proper nutrition, regular exercise, and stress management techniques—can significantly enhance overall well-being. This holistic approach encourages individuals to take a proactive stance toward their mental health by monitoring their symptoms and understanding the triggers in their bodies. Ultimately, seeking help is a vital step in reclaiming control over one’s mental health narrative while addressing the underlying issues related to inflammation and depression.